What is Azoospermia? A General Overview
Azoospermia is a condition in which there are no sperm cells present in a man’s semen. It is often discovered during fertility evaluations following difficulties in conceiving. As one of the most serious and common causes of male infertility, this condition eliminates the possibility of natural conception. Since it usually presents no obvious symptoms, couples often encounter the diagnosis after prolonged unsuccessful attempts to achieve pregnancy. Therefore, being informed about azoospermia and seeking early diagnosis is of great importance.
Types of Azoospermia: Primary vs. Secondary
Azoospermia is categorized into two main types: primary and secondary. Primary azoospermia refers to a congenital absence of sperm production due to impaired testicular function, usually linked to genetic disorders. Secondary azoospermia occurs when sperm production was once normal but ceases over time due to factors such as hormonal imbalances, infections, trauma, or environmental influences.
Distinguishing between these two types is vital for effective treatment planning. While treatment options may be limited in primary azoospermia, it may be possible to restore sperm production in secondary azoospermia by addressing the underlying cause.
Causes: Genetic and Environmental Factors
Many factors can contribute to the development of azoospermia. One of the most frequently encountered causes is genetic abnormalities. Conditions like Klinefelter syndrome and microdeletions on the Y chromosome can impair sperm production and are detectable through genetic testing.
Environmental factors also play a significant role. Exposure to radiation, high temperatures (e.g., in occupational settings), chemical substances, or heavy metals can adversely affect sperm production. Additionally, long-term stress, poor diet, smoking, and alcohol consumption are lifestyle-related contributors that may suppress sperm cell formation.
Diagnostic Methods and Evaluation Process
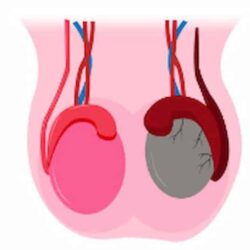
The first step in diagnosing azoospermia is a semen analysis. If no sperm cells are detected in at least two separate samples, further testing is necessary. Hormonal evaluations (including FSH, LH, and testosterone levels) help assess testicular function, while genetic testing can reveal inherited causes.
Scrotal ultrasound is used to examine the size and structure of the testes. In some cases, a testicular biopsy may be performed to determine whether any viable sperm are present. This aids in both diagnosis and treatment decision-making.
Treatment Options and Success Rates
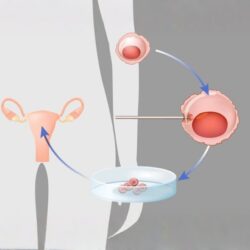
Treatment depends on the type and cause of azoospermia. In cases involving hormonal imbalance, medication therapy may be effective. When obstructions or varicocele are present, microsurgical procedures can be recommended. If sperm production has ceased entirely but rare sperm cells remain in the testicular tissue, microTESE (microsurgical testicular sperm extraction) can be performed for use in assisted reproductive techniques.
Techniques such as IVF (in vitro fertilization) and ICSI (intracytoplasmic sperm injection) offer pregnancy potential even with very limited sperm quantities. Furthermore, lifestyle modifications such as quitting smoking, maintaining regular physical activity, and adopting a healthy diet can enhance treatment outcomes.
Success rates vary depending on the method used, the patient’s age, testicular reserve, and the reversibility of the underlying cause. For this reason, a personalized treatment plan is essential.
Coping with Azoospermia
Azoospermia is a relatively rare but serious cause of male infertility. With early diagnosis and appropriate treatment approaches, many couples struggling with infertility may still have the chance to conceive. Consulting a urologist or reproductive specialist is the first and most critical step toward accurate diagnosis and effective treatment.